AI Billing Team Automation in 2025: Reduce Workload, Boost Speed
Learn how AI billing team automation is easing workloads in 2025 by streamlining tasks, speeding up claims, and improving efficiency in healthcare billing.
4/13/20254 min read

Introduction
“Administrative waste in U.S. healthcare is estimated to cost up to $265 billion annually.” — McKinsey & Company, 2023
That’s a staggering figure—and a large chunk of it stems from outdated, manual billing processes. As someone deeply embedded in the world of medical billing and revenue cycle management (RCM), I’ve seen firsthand how much time billing teams spend on data entry, claim scrubbing, denial rework, and follow-ups.
But that’s changing—and fast.
In 2025, AI billing team automation isn’t just a futuristic concept—it’s a proven, scalable solution that's already lightening workloads and transforming billing operations. Whether you’re a revenue cycle director at a large health system or managing a small clinic, this guide will help you understand how AI is making a measurable impact—with accuracy, compliance, and ROI in mind.
What is AI Billing Team Automation?
At its core, AI billing automation involves using artificial intelligence—particularly machine learning (ML), natural language processing (NLP), and robotic process automation (RPA)—to perform routine billing and revenue cycle tasks.
Here’s how it works in practice:
NLP algorithms extract CPT/ICD codes from physician notes
ML models predict denial risk and flag errors before submission
RPA bots handle repetitive tasks like checking claim statuses and updating ledgers
AI doesn't replace billing staff—it augments them by handling the grunt work, reducing delays, and increasing throughput. This is especially important in 2025, where practices are expected to do more with fewer resources due to ongoing staffing shortages and rising payer scrutiny.
Real-world example: A 2024 HIMSS report showed that clinics using AI-powered coding assistants saw a 27% reduction in claim rejections within 6 months.
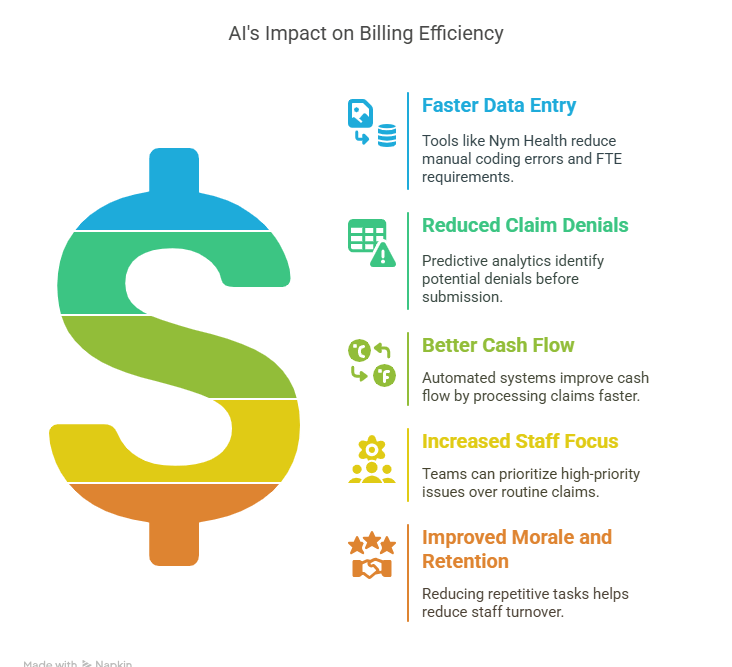
Core Benefits of AI in Reducing Billing Staff Workload
Let’s break this down from a practical, day-to-day operations perspective:
✅ Faster Data Entry & Coding
Tools like Nym Health use NLP to code directly from provider notes—reducing FTE requirements and manual coding errors.✅ Reduced Claim Denials
Predictive analytics highlight claims likely to be denied based on historical payer behavior and documentation issues—before submission.✅ Better Cash Flow
Automated systems process claims faster and reduce days in A/R, improving cash flow. One orthopedic group in Michigan using AI with Waystar reported a 17% drop in average days in A/R within 3 months.✅ Increased Staff Focus on Exceptions & Strategy
Billing teams can shift their time to managing high-priority denials, patient escalations, or compliance audits—rather than chasing routine claims.✅ Morale and Retention
Reducing repetitive workloads helps combat burnout—one of the top drivers of RCM staff turnover today.
Use Cases of AI in Billing Departments
Here are real, current applications of AI in healthcare RCM:
Claim Generation & Submission:
Systems like Olive AI and AthenaIDX automate generation of clean claims, reducing error rates and resubmissions.Denial Prevention & Appeal Automation:
AI flags high-risk claims and generates auto-appeal letters with supporting documentation, cutting appeal cycle times in half.Patient Billing Automation:
Solutions like Cedar Health personalize statements and automate SMS/email reminders, leading to higher patient collections and satisfaction scores.AI Assistants & Chatbots:
Tools like Orbita or Hyro integrate with patient portals to handle FAQs and payment queries, reducing call volume to billing teams.
Best AI Tools for Billing Automation in 2025
From personal experience, the best tools aren't always the flashiest—they’re the ones that integrate seamlessly and support your workflows. Here’s a breakdown of some proven performers:
ToolSpecialtyStrengthsOlive AIEnterprise health systemsWorkflow automation, payer intelligenceWaystarMid to large practicesClaims, denials, and analyticsNym HealthHospitals & clinicsAutonomous medical codingCedarPatient billingUX-focused payment experienceFinThriveRevenue cycle platformPredictive analytics, pre-authorization automation
Features to demand in 2025:
Real-time payer policy updates
Built-in compliance rules (e.g., NCCI edits, LCDs)
Dashboards for denial analytics and A/R forecasting
Interoperability with Epic, Cerner, Allscripts, or Athena
Challenges and Limitations to Be Aware Of
No tool is perfect—and AI has its caveats.
🔐 Data Privacy & Compliance:
Tools must be HIPAA-compliant and HITRUST-certified. Always vet vendors for SOC 2 Type II compliance.💡 Staff Training & Trust:
Teams must understand the “why” behind AI recommendations. Transparency builds trust and usage.🧩 Complex or Ambiguous Cases:
AI may still struggle with unique insurance plans, rare conditions, or unstructured data.📊 ROI Tracking:
Always track impact on KPIs like denial rates, days in A/R, first-pass yield, and FTE reduction.
How to Implement AI Billing Automation Successfully
Here’s a real-world-tested framework I’ve used to guide AI rollouts:
Baseline Your Metrics: Know your denial rates, staff hours per claim, and days in A/R before implementation.
Engage Frontline Billing Staff Early: They’ll help identify broken workflows and vet tool usability.
Run Pilots with High-Volume Claims: Use specialties like primary care or orthopedics to test impact quickly.
Work Closely with Your Vendor: Weekly implementation meetings, training roadmaps, and sandbox testing are a must.
Measure and Iterate: Focus on incremental gains—automating 30% of tasks first is a win.
Future Outlook: How AI Will Reshape Billing Departments by 2030
The RCM landscape is evolving fast. By 2030, we’ll likely see:
End-to-end autonomous RCM – from pre-auth to zero balance
Hyper-personalized patient billing using behavioral analytics
Blockchain-based claims clearinghouses for real-time settlement
AI auditors performing real-time compliance checks during documentation
Billing teams won’t disappear—they’ll shift into higher-skilled roles managing tech, compliance, strategy, and exception handling.
Conclusion
AI is no longer optional in 2025—it’s a competitive edge.
From reducing billing team workload to improving claim accuracy and speed, automation is changing the RCM game. It’s not about replacing your team—it’s about giving them the tools to work smarter, not harder.
If you’re ready to reduce burnout, shorten your revenue cycle, and improve your bottom line—start your AI journey now. Pilot it, measure it, and scale it. Your future team will thank you.