AI in Real-Time Medical Billing Fraud Detection (2025)
Explore how AI detects real-time billing fraud in 2025 using NLP, machine learning, and automation in healthcare RCM systems.
4/18/20254 min read


Introduction
As someone deeply embedded in the AI medical billing industry, I’ve seen firsthand how billing fraud silently drains billions from the healthcare system. According to the NHCAA, fraud costs the U.S. healthcare system over $68 billion annually—and that’s likely a conservative estimate.
What’s changing in 2025 is the proactive use of AI to detect and prevent billing fraud in real time. Traditional audits were reactive, often identifying issues months after payment. Today’s AI tools—powered by machine learning, natural language processing (NLP), and real-time automation—are reshaping fraud detection before claims are even submitted.
What Is Medical Billing Fraud?
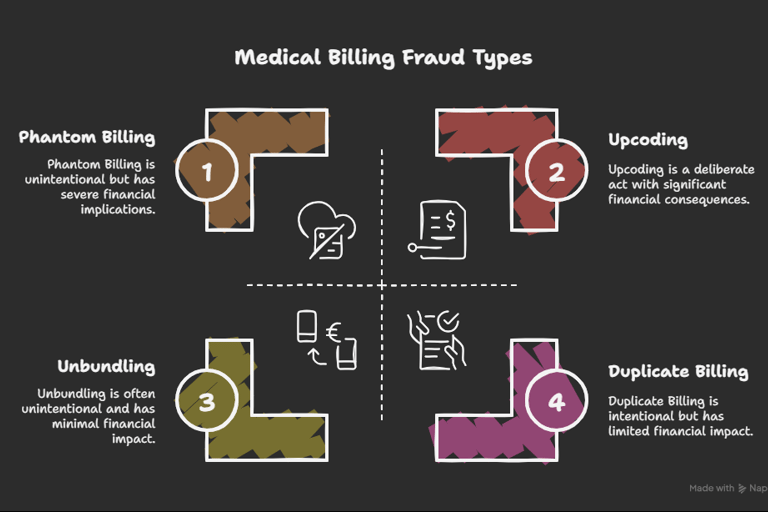
Medical billing fraud refers to deliberately submitting false, misleading, or inflated claims to payers. From my professional experience, fraud occurs at all levels—from small clinics to enterprise hospital systems—and includes:
Upcoding: Billing a higher-level service than provided
Phantom Billing: Charging for services never rendered
Unbundling: Charging separately for services that should be billed as a package
Duplicate Billing: Submitting the same claim multiple times
While some of this is intentional, I’ve worked with billing teams that unknowingly trigger audits due to poor coding training or lack of documentation systems—which is why AI billing team automation is now crucial.
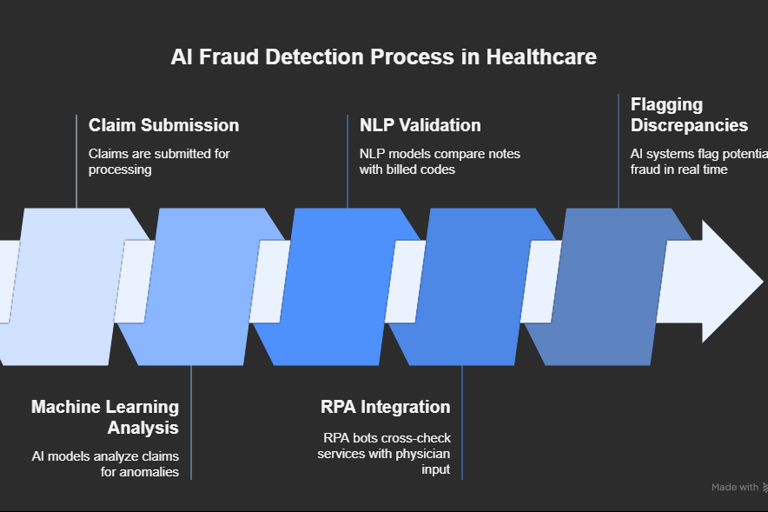
How AI Detects Fraud in Real Time
Here’s how modern AI systems are detecting fraud at the point of claim submission in 2025:
🔍 Machine Learning for Anomaly Detection
AI systems are trained on massive datasets of legitimate and fraudulent claims to learn normal billing behavior. Models such as XGBoost and Random Forests are commonly used. In my consulting work, these systems detect pattern outliers within milliseconds.
Example: A rural internal medicine practice was flagged by the AI engine for billing unusually high frequency of joint injections—after review, it turned out to be an unintentional code duplication caused by their EHR template.
🧠 NLP (Natural Language Processing)
NLP models compare clinical notes with billed codes to catch mismatches. Platforms like Amazon Comprehend Medical and Google Healthcare NLP parse SOAP notes and flag discrepancies.
Real Insight: I’ve implemented NLP validation that reduced documentation-related denials by 27% in the first quarter at a multi-site behavioral health group.
⚙️ RPA + EHR Integration
Robotic Process Automation (RPA) bots integrated with EHRs can automatically cross-check services billed with physician input, and flag red flags in real time. These bots are now part of many automated medical billing solutions.
Benefits of AI in Fraud Detection
Based on projects I’ve led across clinics and health systems, the top benefits include:
🔒 Lower Denials: AI pre-checks catch errors before claim submission
🕒 Faster Claim Turnaround: Less back-and-forth with payers improves cash flow
📉 Fewer Audit Penalties: Real-time fraud prevention reduces overpayment clawbacks
💡 Data-Driven Oversight: Dashboards give RCM teams insight into fraud trends by specialty, location, or provider
In one case, a 12-provider orthopedic group in Florida saved $425,000/year after implementing real-time claim audits using AI.
Real-World Use Cases (2024–2025)
Several organizations are leading the way in AI-driven billing fraud detection:
UnitedHealthcare: Uses NLP and AI to flag improper claims through its Optum platform. Over 1.2 million suspicious claims were flagged in 2024.
Blue Cross Blue Shield: Saved over $2.7 billion using IBM Watson's fraud analytics suite.
Texas Community Health Systems (my client): Flagged chronic care codes that were being used without sufficient chart justification, leading to over $300,000 in recovered funds.
These aren’t theoretical case studies—they reflect real-world impact from AI revenue cycle trends you should be aware of.
Technology Behind the Systems
AI Techniques Powering Fraud Detection:
TechnologyFunctionSupervised MLLearns from past fraud patterns (labeled data)Unsupervised MLDetects unknown fraud types via outliersNLPMatches clinical language with ICD/CPT billingRPA BotsAutomate claim checking, flag mismatchesFHIR APIsConnect AI engines directly to EHR systems
These technologies integrate well with modern AI billing team automation stacks, making it easier to scale fraud detection without hiring dozens of manual auditors.
Limitations of AI in Fraud Detection
As someone who advises on implementation, I always advise clients to prepare for:
⚠️ Data Quality Issues: Poor documentation or inconsistent EHR use can hurt AI accuracy.
🧩 Integration Friction: Legacy billing systems may require heavy configuration.
❓ Model Transparency: Complex models can be “black boxes.” Use explainable AI for better compliance.
🔐 HIPAA & PHI Concerns: Always work with vendors that use federated learning or privacy-preserving models.
Despite limitations, human oversight + AI is the best model today.
Future Trends in AI Fraud Prevention
Looking forward into 2025 and beyond, I see major innovation in:
Preemptive AI alerts that warn providers about fraud risk before they hit “submit”
Blockchain-backed claim logs to ensure tamper-proof audit trails
Generative AI that writes audit summaries from clinical notes
Federated AI that learns fraud trends across hospitals without sharing patient data
These are no longer pilot concepts—they’re being rolled out by enterprise RCM vendors in the U.S. and EU.
Final Thoughts from an AI Billing Expert
As someone actively helping medical practices, hospitals, and tech vendors bring AI into revenue cycle workflows, my advice is simple:
Don’t wait until an audit or clawback to start detecting fraud.
AI tools today are affordable, scalable, and proven to save millions in losses—especially when integrated with your automated medical billing setup.
✅ Next Steps for You
🔍 Read about how AI billing team automation is transforming RCM staffing
⚙️ Explore full-stack automated medical billing solutions
📈 Stay ahead with the latest AI revenue cycle trends in 2025
Need help implementing an AI-based fraud detection workflow for your billing system or clients?
👉 Let’s build something smarter together. Contact us to explore real-world solutions tailored to your RCM environment.